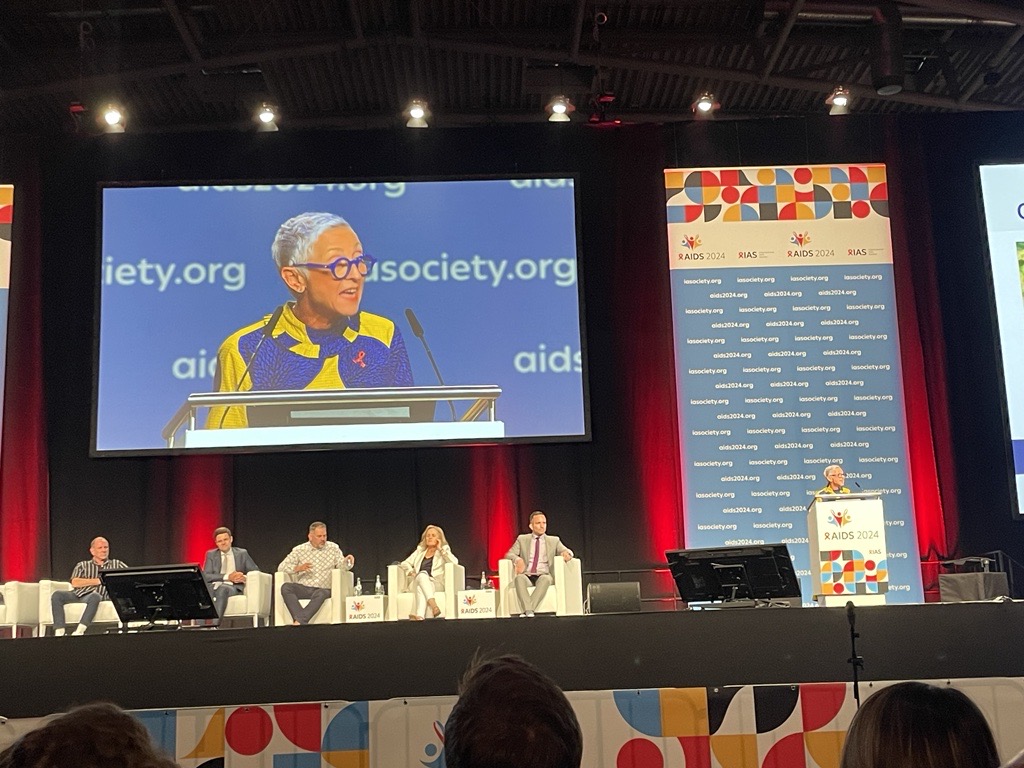
MUNICH – Delegates at the International AIDS conference leapt to their feet in delight after results from one of the most promising HIV prevention trial in the history of the epidemic – a twice-yearly injection of lenacapavir that prevented 100% of new HIV infections – were presented on Wednesday.
Principal investigator Professor Linda-Gail Bekker from South Africa told the conference that none of the 2,134 women aged 16 to 25 who had received lenacapavir on the PURPOSE 1 trial contracted HIV.
The results, also published in the New England Journal of Medicine, compared the injectable lenacapavir with two regimens involving daily pills that have previously proven to be effective as HIV pre-exposure prophylaxis (PrEP).

However, by the end of the trial, the 3,204 women in the two pill groups reported HIV cases similar to projected population-based HIV acquisition – not because the pills didn’t work but because participants’ adherence was “low”.
Young people generally find it difficult to take daily pills because they fear being questioned about it, according to another trial from Uganda due to be presented at the conference.
Describing the results as “stellar”, Bekker said that the medicine offers “a highly effective, tolerable and discreet choice that could potentially improve PrEP uptake and persistence, helping us to reduce HIV in cisgender women globally”.

“PURPOSE 1 also sets a new standard for person-centered HIV prevention trials, demonstrating what can happen when a thoughtful scientific and community-focused trial design, a promising drug candidate and an inclusive trial implementation plan come together,” added Bekker, who is director of the Desmond Tutu HIV Center at the University of Cape Town.
Results from the PURPOSE 2 trial testing lenacapavir in men, transgender and non-binary people who have sex with men in Argentina, Brazil, Mexico, Peru, South Africa, Thailand and the US is expected by early 2025.
International AIDS Society president Sharon Lewin described the trial results as “a breakthrough advance with huge public health potential”.

“If approved and delivered – rapidly, affordably, and equitably – to those who need or want it, this long-acting tool could help accelerate global progress in HIV prevention. We all owe a debt of gratitude to the thousands of young women in South Africa and Uganda who volunteered to be part of this study,” said Lewin.
Gilead under pressure to lower price
HIV leaders, activists and researchers have called on lenacapavir producer Gilead to make its medicine widely accessible.
“We still have 1.3 million new HIV infections per year. UNAIDS wants this ‘miracle’ prevention drug to reach all those who need it, now, not in six years’ time,” said UNAIDS executive director Winnie Byanyima at a media briefing on Wednesday.
She urged Gilead to “move quickly to licence lenacapavir to generic producers” via the Medicines Patent Pool.
“Generic producers bring prices down and serve all countries where the majority of people who are at risk live,” added Byanyima.
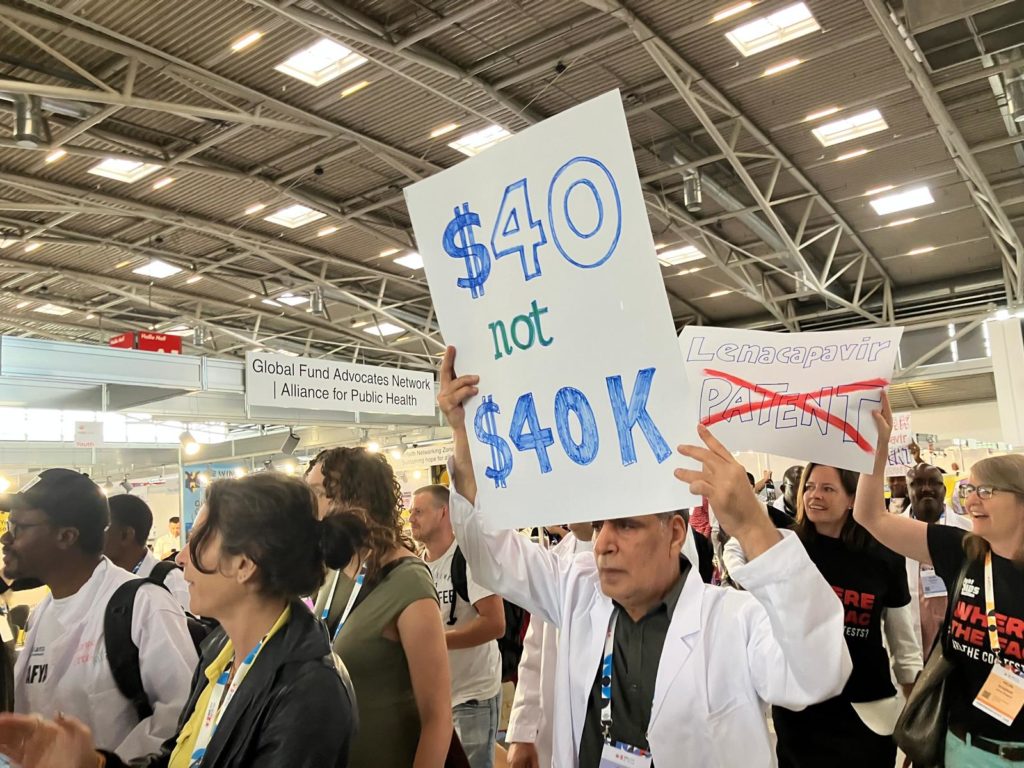
On Tuesday, activists protested at Gilead’s conference booth demanding that the company make the medicine 100% accessible.
At present, lenacapavir is licensed in the US as Sunlenca for people with drug-resistant HIV and sells for $42,000 a year – yet generic companies can make it for as little as $40, according to research conducted by Dr Andrew Hill.
By Health Policy











